Navigating Comprehensive Dental Care for Cleft Palate: A Multidisciplinary Approach
In the journey toward optimal oral health for individuals with specific facial challenges, coordinating multiple aspects of treatment is essential. Emphasizing a harmonized approach from an early age can significantly influence overall outcomes, paving the way for enhanced function and appearance through diligent planning and expert care.
Orchestrating the Medical Journey
The Importance of a Coordinated Start
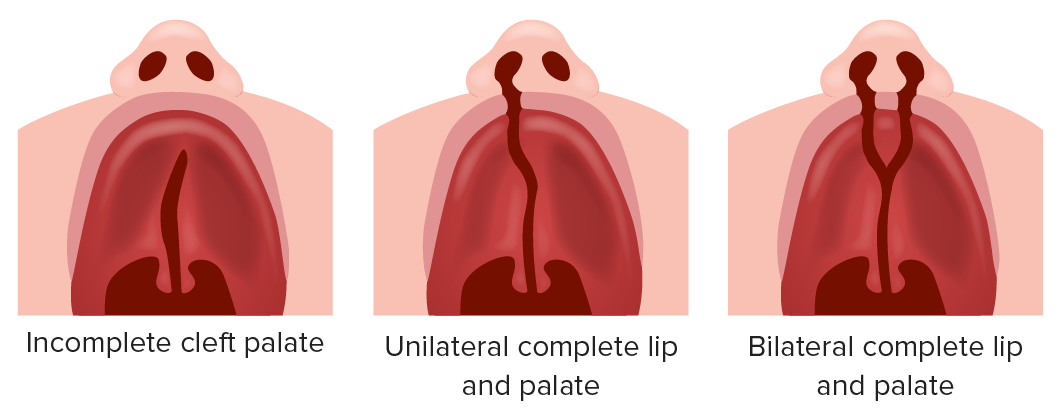
Treating congenital craniofacial differences goes far beyond cosmetic adjustments; it is a profound medical discipline aimed at fundamental functional restoration. Unlike general dentistry, where practitioners monitor standard developmental milestones, care for these specific conditions requires a deep understanding of unique structural anatomies from birth. In clinical settings, the approach involves a meticulous comparison against standard growth data while maintaining a long-term perspective. Because the timing of tooth eruption and the velocity of jaw growth vary significantly among these patients, a one-size-fits-all methodology is ineffective. Instead, a highly personalized analysis tailored to each growth stage is indispensable for success.
The cornerstone of effective management lies in the seamless collaboration between various specialties, particularly orthodontics and oral surgery. This is not a solitary path but a collective effort. For instance, addressing a deficit in jaw bone volume often requires surgical intervention, which must be perfectly timed with orthodontic preparations to create a solid foundation for future restorative work or implants. Experienced professionals in this field do not view straight teeth as the ultimate goal. Rather, they strategize based on how the entire jaw alignment interacts with speech capabilities and respiratory function. By adopting this comprehensive mindset, complex dental challenges are unraveled step by step, steadily elevating the patient's quality of life.
Crucially, "early intervention" in this context signifies more than just early surgery. It represents a proactive strategy that begins almost immediately after birth. Specialists from neonatology, pediatrics, and oral surgery unite to formulate a roadmap that anticipates future growth spurts. Recent clinical data suggests that receiving such integrated care from infancy can reduce the severity of future surgical needs and lead to more natural facial aesthetics. for families, knowing that a dedicated team is monitoring their child’s development provides a significant layer of psychological comfort and reassurance amidst the uncertainties of treatment.
Restoring Function Through Advanced Devices
How Custom Apparatuses Aid Daily Life
In the comprehensive treatment landscape, prosthetic devices play a role just as critical as surgical procedures. These are not merely passive tools; they are active facilitators of daily function. For many patients, specifically designed appliances—often referred to as obturators or speech aids—are custom-fabricated to fit the unique contours of the mouth. Their primary function is to physically bridge gaps in the palate that surgery may not have fully closed or to assist before surgery is viable. By effectively sealing the oral cavity from the nasal passage, these devices prevent air leakage, which is the primary culprit behind hypernasal speech. Furthermore, they drastically improve the ability to create suction and pressure, which are vital for efficient swallowing and chewing.
The manufacturing process of these essential tools has undergone a revolution thanks to digital technology. Historically, creating these devices involved filling a child’s mouth with impression material—a process that could be uncomfortable and distressing. Today, the adoption of intraoral scanners allows practitioners to capture precise digital topographies of the mouth without physical contact. This data is then used to design devices with micron-level accuracy, which are subsequently produced using 3D printing technologies. This shift not only alleviates physical stress for the patient but also reduces the number of visits required for adjustments.
Material science has also advanced, introducing flexible resins and biocompatible silicones that offer superior durability and comfort. A device is only effective if it is worn, and these modern materials ensure that patients can wear their appliances for extended periods without irritation. When these devices are integrated effectively, patients report immediate improvements in speech clarity and dietary variety. However, the mouth is a dynamic environment that changes with age. Therefore, continuous collaboration with prosthodontists and speech therapists is necessary to adjust or replace these devices, ensuring they evolve alongside the patient’s growth.
| Feature | Traditional Fabrication Method | Digital & 3D Printed Method |
|---|---|---|
| Impression Process | Requires physical putty/mold in the mouth, which can cause gagging or anxiety. | Uses a handheld scanner wand for a touch-free, rapid digital image capture. |
| Precision & Fit | High quality, but subject to material shrinkage or manual handling errors. | Extremely high precision based on exact data coordinates; highly reproducible. |
| Patient Comfort | Materials can be bulky or rigid; adjustments require manual grinding. | Allows for thinner, lighter designs using flexible, biocompatible materials. |
| Turnaround Time | Slower due to physical shipping of molds and manual lab work. | Faster production cycles; data is sent instantly to 3D printers or milling machines. |
Aligning Smiles and Speech Mechanics
Phased Orthodontic Interventions
Orthodontic care for patients with cleft conditions is distinct from cosmetic straightening; it is a strategic, multi-phase medical necessity that spans from childhood into early adulthood. The treatment timeline is dictated strictly by the patient's biological clock rather than chronological age. One of the most critical phases occurs during the transition from primary to permanent teeth, often around early elementary school age. During this window, the focus shifts from simple alignment to structural expansion. The primary objective is often to widen the upper jaw and correct the dental arch's shape to prepare for secondary procedures.
A pivotal moment in this timeline is the preparation for the alveolar bone graft. This surgical procedure involves transplanting bone to the gum line to fill the cleft, providing a solid matrix for permanent teeth—specifically the canines—to erupt into. Orthodontists play a vital role here by expanding the dental arch to ensure the gap is accessible and the surrounding teeth are positioned to support the graft. If the arch is not properly shaped, the graft may fail to integrate, or the permanent teeth may not have adequate room to descend.
This symbiotic relationship between the orthodontist and the surgeon highlights the need for a long-view approach. Every bracket placed and every expander turned is a calculated move to facilitate a future surgery or prevent a future complication. Families are encouraged to view this as a marathon. Regular monitoring allows the team to intercept problems, such as crossbites (where the top teeth sit inside the bottom teeth), before they impact skeletal growth permanently. This phased approach ensures that when the child reaches skeletal maturity, the foundation is set for the final alignment, minimizing the severity of orthognathic (jaw) surgery if it becomes necessary.
The Symbiosis of Sound and Structure
There is an intrinsic link between the architecture of the oral cavity and the ability to articulate sound. One can think of the mouth as a musical instrument; if the shape of the instrument is altered, the resonance and clarity of the notes change regardless of the musician's skill. For children born with clefts, the "instrument" often has structural irregularities—such as gaps in the dental row, a fistula in the palate, or misalignment of the jaws—that make producing specific sounds physically impossible. Sounds like "s" and "t," which require the tongue to make a precise seal against the alveolar ridge (the gum area behind the top teeth), are particularly vulnerable to distortion if that ridge is irregular or if teeth are missing.
Therefore, dental and orthodontic correction is often a prerequisite for successful speech therapy. No amount of speech practice can fully correct an articulation error caused by air escaping through a dental gap. This is why the dental team and speech-language pathologists must work in lockstep. For instance, an orthodontic expander might temporarily alter tongue placement, making speech more difficult for a few weeks. Conversely, successful expansion might suddenly provide the tongue the room it needs to articulate sounds that were previously muffled.
The treatment plan must be fluid, adapting to these changes. A speech therapist might request specific dental movements to aid articulation, while a dentist might delay certain procedures to prioritize speech milestones. This holistic view acknowledges that "fixing the teeth" is not just about a visual smile—it is about giving the child the physical capability to communicate clearly. By normalizing the oral structure, the medical team removes the physical barriers to speech, allowing the child’s personality and voice to shine through without the hindrance of articulation difficulties.
A Lifetime of Confidence and Health
Beyond the Surgery: Holistic Support
While the technical aspects of surgery and dentistry are vital, the ultimate measure of success in treating cleft lip and palate is the patient's long-term quality of life. The medical journey does not end when the braces come off or the final suture heals. It is a pathway that extends well into adulthood, requiring a support system that evolves as the patient matures. Modern care centers emphasize a "whole-person" philosophy. This means that alongside monitoring gum health and jaw stability, the care team pays close attention to nutritional intake, psychosocial well-being, and educational integration.
For children, having a visible facial difference can impact social interactions and self-esteem. Therefore, the dental and surgical teams often integrate psychological support into the care plan, helping children navigate the social challenges of school and adolescence. As patients transition into adulthood, the focus shifts toward maintaining the results achieved during childhood. Adult patients require education on how to care for implants, bridges, or surgically reconstructed areas, which may be more susceptible to gum disease or decay than typical oral structures.
Furthermore, the aggregation of long-term data is reshaping how care is delivered. By analyzing the life-long outcomes of thousands of patients, medical communities are refining their techniques to reduce the burden of care. Today’s treatments are less invasive and more effective because they stand on the shoulders of decades of research. This cycle of continuous improvement ensures that the "tailored" care received by a child today is scientifically designed to maximize their future well-being, ensuring that their smile remains healthy and confident for decades to come.
| Growth Stage | Primary Care Focus | Goal of Intervention |
|---|---|---|
| Infancy & Toddlerhood | Feeding support, lip repair, and initial palate closure. | Ensuring proper nutrition/weight gain and establishing a separation between nose and mouth for speech. |
| Early Childhood (Ages 6-9) | Expansion orthodontics and speech therapy. | Widening the upper jaw to prevent crossbite and preparing the bone gap for grafting; refining articulation. |
| Pre-Adolescence (Ages 9-12) | Alveolar bone grafting and monitoring canine eruption. | uniting the gum ridge with bone to allow permanent teeth to erupt and stabilizing the dental arch. |
| Adolescence to Adulthood | Comprehensive orthodontics and final jaw surgery (if needed). | Achieving the final aesthetic bite, ensuring long-term stability, and transitioning to adult maintenance care. |
Q&A
-
What is the role of multidisciplinary care teams in managing cleft conditions?
Multidisciplinary care teams are essential in managing cleft conditions as they bring together various specialists such as surgeons, orthodontists, speech therapists, and prosthodontists. This collaborative approach ensures comprehensive treatment planning and care, addressing the complex needs of individuals with clefts. Each specialist contributes their expertise, allowing for coordinated treatment that improves functional and aesthetic outcomes.
-
How does early oral rehabilitation benefit patients with cleft conditions?
Early oral rehabilitation is crucial for patients with cleft conditions as it helps in promoting normal oral development and function. By initiating treatment at an early stage, healthcare providers can address issues such as feeding difficulties, speech development, and dental anomalies. This proactive approach can significantly improve the quality of life for patients and reduce the complexity of future treatments.
-
What role does prosthetic dentistry play in the treatment of cleft conditions?
Prosthetic dentistry is vital in the treatment of cleft conditions, as it provides solutions for missing or malformed teeth, often associated with clefts. Prosthodontists design and fit dental prostheses that restore function and aesthetics, contributing to improved oral health and self-esteem for patients. These prostheses can also aid in speech development and proper alignment of the jaw and teeth.
-
Why is orthodontic preparation important in the treatment of cleft conditions?
Orthodontic preparation is important in cleft treatment as it prepares the teeth and jaws for surgery and prosthetic interventions. Orthodontists work to align teeth and correct bite issues, which can be crucial for the success of surgical procedures and the overall treatment plan. Proper orthodontic preparation can lead to better functional and aesthetic outcomes for patients.
-
How does long-term treatment planning benefit individuals with cleft conditions?
Long-term treatment planning is beneficial for individuals with cleft conditions as it provides a roadmap for ongoing care and intervention. This approach anticipates future needs and adjustments, allowing for timely interventions that can prevent complications and optimize outcomes. A long-term plan helps ensure that patients receive consistent care throughout their development, addressing changes in dental, speech, and facial growth over time.
